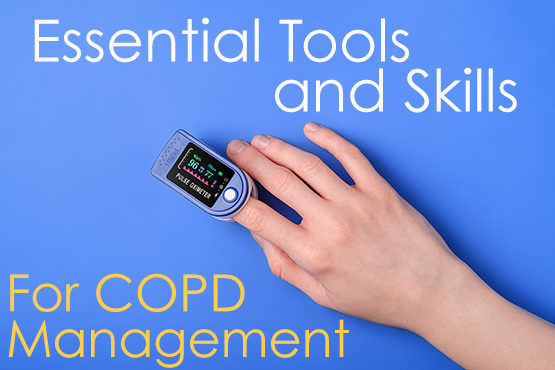
Pulse Oximeters: Essential Disease Management Tool for Respiratory Patients
Respiratory diseases, including Chronic Obstructive Pulmonary Disease (COPD), asthma, pulmonary fibrosis, and others, affect millions worldwide. Proper disease management requires vigilance and proactive care to prevent complications and improve quality of life.
What is Respiratory Disease Management?
The ultimate goal of disease management is to slow disease progression. Conditions like COPD, Pulmonary Fibrosis, and IPF are progressive diseases, meaning that severity can grow over time. However, just because you may have been diagnosed with something for which there is no cure, that doesn’t mean that nothing can be done to slow disease progression and maintain quality of life.
Essential disease management includes:
- Taking Medication as Directed and Prescribed – Take medication as directed and never stop taking a medication without speaking to your doctor. If you are experiencing side effects, discuss it with your doctor, they may be able to adjust the dosage or way you take it to decrease negative effects.
- Lifestyle Changes – Quitting smoking, increasing physical activity, and improving eating habits can all contribute to slowing disease progression and decreasing symptoms.
- Keeping a Food Diary – Eating healthy is important for everyone but it’s important to know which foods negatively affect your breathing. It may be because they cause bloating which causes your stomach to press up against your diaphragm, making it hard to breathe. It could also be that the food causes an allergic reaction, or it just may be food that doesn’t agree with you. Keeping a food diary will help you to identify these foods. It will also be useful to show the diary to your doctor and nutritionist to help them better understand your eating habits.
- Monitoring Symptoms – An uptick in symptoms such as coughing, mucus production, and shortness of breath can be an early indicator of an exacerbation. A serious exacerbation can land you in the hospital and nothing will speed up disease progression like a serious respiratory virus. Close symptom observation can allow you to get help before an exacerbation becomes serious and results in a hospital stay.
- Keeping Track of Oxygen Saturation Levels – Oxygen saturation levels is the measurement of how much oxygen is in your blood. Every cell, organ and tissue in your body requires oxygen to function properly. If your saturation levels are consistently below normal levels, this is a condition called hypoxia.
Get Your Free Respiratory Symptom Monitoring Action Plan!
Click Here to get our FREE symptom monitoring sheet. It’s easy to follow along each day and identify symptom escalation which may indicate a coming exacerbation. Our COPD action plan form also provides a convenient place to record what medication you are on, when you take them, insurance information and other vital info you may need if you end up in the emergency room.
You may think that this is unnecessary because you know this information but keep in mind that if your saturation is low you may be disoriented and not thinking clearly. Share this info with a neighbor, spouse, and emergency contact so they can access that information in an emergency.
Symptoms of Hypoxia
Consistently low oxygen levels can cause organ and tissue damage as well as cellular impairment. Over a long period damage can become permanent or in severe cases, coma, loss of brain function, or even death can occur.
Symptoms of Low Saturation Levels or Hypoxia Include:
- Shortness of Breath
- Dizziness
- Rapid Heart Rate
- Shallow and Rapid Breathing
- Confusion
- Headache
- Chest Pain
- Weakness
- Poor Coordination
- Bluish Tint to Fingertips or Lips
Monitoring Oxygen Saturation
Keeping a close eye on saturation levels is essential to proper disease management. Consistently dropping oxygen levels can have serious consequences. Luckily monitoring saturation is easy and convenient with a device called a pulse oximeter.
A pulse oximeter is a vital, inexpensive, and easy-to-use management tool for respiratory patients, offering real-time insights into blood oxygen levels and enabling timely interventions.
What is a Pulse Oximeter?

A pulse oximeter is a compact, non-invasive device used to measure blood oxygen saturation levels and pulse rate. It works by passing light through a part of the body, typically a fingertip, earlobe, or toe, and calculating the percentage of oxygen in the blood based on the absorption of light.
For individuals with compromised lung function, such as those with COPD, asthma, or interstitial lung disease, monitoring oxygen saturation is critical. Persistent low oxygen levels can lead to serious exacerbation and increased disease progression, making real-time monitoring indispensable.
Why Pulse Oximeters Are Essential for Respiratory Patients
1. Early Detection of Low Oxygen Levels
Patients with respiratory diseases are at higher risk of hypoxemia, a condition characterized by insufficient oxygen in the blood. A pulse oximeter provides immediate feedback, alerting patients if their oxygen levels fall below safe thresholds. For most individuals, normal oxygen saturation (SpO₂) levels range between 95-100%. However, those with chronic respiratory conditions might have acceptable levels as low as 88-92%, as determined by their healthcare provider.
2. Prevention of Exacerbations
Respiratory conditions can worsen suddenly due to infections, allergens, environmental pollutants, or other triggers. A sudden drop in saturation levels can indicate an impending exacerbation. By identifying these changes early, patients can seek timely medical care, reducing the severity and frequency of hospitalizations.
3. Optimization of Oxygen Therapy
For patients using supplemental oxygen, whether via a portable oxygen concentrator or home oxygen system, a pulse oximeter ensures your oxygen flow prescription is adequate. It allows for adjustments based on activity levels, ensuring proper oxygenation during rest, exercise, or travel.
4. Enhanced Self-Management
Managing a chronic respiratory condition often involves tracking symptoms, triggers, and treatments. A pulse oximeter provides objective data that can be logged and shared with healthcare providers. This data enables more personalized care plans and helps patients feel more in control of their condition.
5. Improved Quality of Life
Knowing that oxygen levels are within a safe range provides peace of mind, encouraging patients to engage in daily activities and exercise. This sense of security can be very empowering, and significantly enhance overall well-being and independence.
Watch this Video to Learn How to Take an Oxygen Saturation Reading Effectively!
Best Practices for Using a Pulse Oximeter
To maximize the benefits of a pulse oximeter and ensure accurate readings, follow these best practices
Understand Your Target Oxygen Saturation Levels
- For healthy individuals, normal levels are 95-100%.
- For those with respiratory conditions, acceptable levels may differ. Always consult your healthcare provider for individualized guidance.
Best Practices for Taking a Saturation Reading
- Rest for a few minutes before taking a reading.
- Ensure your hands are warm and relaxed before measurement. Cold extremities or poor circulation can result in inaccurate readings.
- Sit still and avoid moving your had during measurement
- Remove nail polish or artificial nails, as they can interfere with the device’s light sensor.
- Read in regular room light. Bright sunlight can affect the accuracy of your reading.
- Check levels at the same time of day for consistency.
Monitor Regularly
- Check oxygen levels if you have unusual activity levels or weather to see what causes your oxygen levels to shift.
- For those using supplemental oxygen, monitor oxygen saturation levels to confirm the adequacy of oxygen therapy.
Record and Share Your Data
- Maintain a log of your saturation readings, noting the date, time, activity level, and any accompanying symptoms.
- Bring your result log with you to your doctor’s appointments. Seeing results trending or fluctuating can give your doctor valuable insight into your condition so that they can make informed decisions regarding adjusting your medications or other directives.
Recognize When to Seek Medical Help
If oxygen levels drop consistently over a period of days or drop suddenly, this could be a sign of an exacerbation coming on. Speak with your doctor about your readings and ask what trends or readings should trigger a call to the doctor and what trends or readings should trigger an immediate trip to the hospital.
Integrating Pulse Oximetry with Other Tools

Pulse oximeters can be paired with other devices to create a comprehensive respiratory management plan. Here’s how they complement other tools:
Portable Oxygen Concentrators
-
-
- Adjust Oxygen Levels: Pulse flow settings can vary with different oxygen concentrator manufacturers. Use a pulse oximeter to ensure you are properly titrated at the level that your doctor has prescribed.
- Monitor During Travel: Altitude changes and increased exertion can affect oxygen needs. A pulse oximeter ensures your oxygenation remains stable during trips.
- Assess Sleep Oxygenation: Monitor overnight oxygen levels to evaluate the effectiveness of supplemental oxygen during sleep. If you wake up feeling out of breath, confused, or otherwise out of sorts, take your saturation reading.
-
Preventing Exacerbations Through Proactive Monitoring
Proactive use of a pulse oximeter can help minimize the risk of exacerbations by:
-
-
- Monitoring Environmental Triggers: Track oxygen levels when exposed to potential triggers like smoke, allergens, or extreme temperatures. If oxygen saturation drops, take steps to mitigate exposure or increase oxygen therapy as advised.
- Encouraging Medication Adherence: Saturation readings can act as a visual cue to stay consistent with prescribed inhalers, nebulizers, or other treatments.
-
Choosing the Right Pulse Oximeter
When selecting a pulse oximeter, consider the following features:
-
-
- Ease of Use: Devices with a clear display and one-button operation are best for ease of use..
- Portability: Compact, lightweight designs are ideal for daily use and travel.
- Additional Features: Advanced models with Bluetooth connectivity allow data syncing with smartphones making detailed tracking and reporting easier.
-
Proper Respiratory Management with a Pulse Oximeter
A pulse oximeter is more than a monitoring device; it’s a tool for empowerment and improved care. For patients with respiratory diseases, regular use of a pulse oximeter provides critical insights that enable early intervention, optimize oxygen therapy, and prevent exacerbations. Combined with other management strategies, it enhances quality of life and reduces the risk of complications.
Whether you or a loved one is living with COPD, asthma, or another respiratory condition, incorporating a pulse oximeter into your routine can make a significant difference. With consistent monitoring and proactive care, better respiratory health is within reach.
Optimize Your Respiratory Health Today
Explore high-quality pulse oximeters and supplemental oxygen devices tailored to your needs. Take charge of your respiratory care and breathe easier, every step of the way.
If You’ve Just Been Prescribed Oxygen, We Can Help!

If you’ve been experiencing symptoms of hypoxia, you’ve likely been given a pulmonary fit test. Those with oxygen saturation levels were consistently under 90% during certain times or activities, you may have been told that you need supplemental oxygen.
While this news can be scary and unsettling at first, the truth is that when you begin oxygen therapy and your saturation levels normalize, you’ll probably feel better and have more energy than you have in a very long time!
Our respiratory team can help you find the perfect portable oxygen concentrator for your medical needs. If you’re on Medicare, they’ll ensure that you get all the benefits and financial assistance to which you are entitled. If you’re paying out of pocket we have several financing options available. Give us a call today at 888-643-4921!
Don’t forget to get your FREE COPD Action Plan Sheet – CLICK HERE!



0 Comments